Borderline Personality Disorder – a label with history and her-story behind it
September 9th, 2015 | Published in Favorites, Health & Mental Health
“As a young adult,” Ann Kennedy writes (personal communication), “they gave me the label of Borderline Personality Disorder.”
 Years later, when she was able to access her medical records, Ann found no mention of bullying and tyranny in her family of origin, and the sexual abuse by her much older brother was written off in a single comment. The cutting and burning she self-inflicted when “the mental and emotional pain became unbearable” was undocumented except to call her “an attention seeker”.
Years later, when she was able to access her medical records, Ann found no mention of bullying and tyranny in her family of origin, and the sexual abuse by her much older brother was written off in a single comment. The cutting and burning she self-inflicted when “the mental and emotional pain became unbearable” was undocumented except to call her “an attention seeker”.
Medication was the treatment. She refused ECT.
After living with her label for 28 years, Ann sold an heirloom and was able to pay for private therapy. Within six months she had stopped self-mutilating. She began to develop an understanding of why she behaved the way she did, why she saw other people and the world as dangerous, and why she thought of herself as worthless, stupid, and inconsequential.
Ann goes on to describe her work as an artist, illustrator, and writer. “Today,” she says, “I am living a life that is satisfying and understandable.”
Why this subject?
I am writing about BPD because I was asked to, and I said I would, even though I knew at the time how hard it would be. The term itself begs questions that are part of the discussion.
I understood that those who made the request did so for  personal reasons, and I wanted to honour that. One thing not in dispute is the pain and suffering of people diagnosed, or the challenges for those who support them.
personal reasons, and I wanted to honour that. One thing not in dispute is the pain and suffering of people diagnosed, or the challenges for those who support them.
Many people have much to say about this topic. A google search yields 7,660,000 results, considerably more than Narcissistic Personality Disorder (1,330,000), although fewer than Schizophrenia (23,100,000) or Depression (218,000,000).
There is clearly nothing new to say and too much to synthesise, but some issues that can frame the material include the gendered history of the diagnosis; the connections to developmental trauma; the distinction between insider and outsider perspectives; and the effect of perspective on description of symptoms, choice of models and treatments.
A diagnosis with history and her-story behind it
Women have traditionally been much more likely than men to be diagnosed with BPD. In clinical psychiatric settings 75% of cases are women, men being more likely to show up in prisons or drug services (see, for example, here, and here).
Approximately 80% of those diagnosed with BPD have a history of trauma associated with childhood abuse, although the term itself gives no suggestion of either the gender skew or links with developmental history. It is effectively a reductionist label that airbrushes the social conditions that produce the symptoms it describes (see here, here, and here).
of trauma associated with childhood abuse, although the term itself gives no suggestion of either the gender skew or links with developmental history. It is effectively a reductionist label that airbrushes the social conditions that produce the symptoms it describes (see here, here, and here).
Interestingly, Narcissistic Personality Disorder (NPD) has the opposite gender balance, being more often diagnosed in men than women. Its criteria include sense of entitlement, arrogance, fantasies of power, and grandiosity – characteristics associated with cultural constructions of masculinity.
BPD, with its diagnostic symptoms of dependency, insecurity, sensitivity, and fragility is more aligned with cultural constructions of femininity.
The overlap of NPD with masculinity, and BPD with femininity, raises questions about these diagnoses (among others) that take them beyond the realm of individual pathology into the sociopolitical context of gender and power relations.
The prerogative to name someone else’s experience is, after all, an exercise of social power. The more marginalised a person is in terms of gender, race, class, sexuality, able-ness, and other dimensions, the less power they have to contest the way they are labelled.
Working with asylum seekers, for example, I have frequently challenged the way labels, including BPD, are applied. Of course people are overwhelmed, and have trouble regulating their impotent anxiety and fear for the future. But, their problem is first and foremost their toxic circumstances rather than some free-floating personal pathology.
In sum, the behaviors labelled BPD need to be understood in the context of social power including, importantly, gendered power. They also need to be understood against the backdrop of the person’s developmental history, as Ann Kennedy’s story of sexual and other abuses in her family of origin illustrates.
Outsider-Insider viewpoints
Much of the available material on BPD comes from outsider perspectives – mental health practitioners, researchers and journalists, for example, who don’t have the diagnosis themselves, or at least don’t state that they do. A smaller volume of material is from those inside the experience, and some of that is addressed to those outside it.
The outside-inside distinction is particularly important in the case of BPD because of the extreme stigma associated with it (see here, and here).
Gunn and Potter, for example, recall a conference at which Irvin Yalom, a well-known psychiatrist, was asked if he still works with clients (having been around for decades).
“Well,” he said “I’m not taking any borderline clients.”
This response was hugely funny to those at the conference, apparently, consistent as it is with the recommended way of dealing with BPD – by referring people on (see here).
An outsider (like Yalom) might see a person who ‘acts out’, ‘seeks attention’, ‘is manipulative’ and recurrently ends up in emergency departments; someone, that is, who is not a ‘good patient’.
The inside experience, on the other hand, is likely to be of 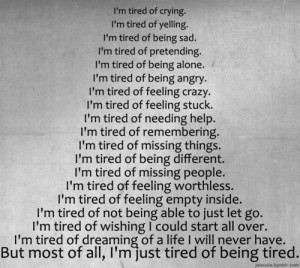 overwhelming psychic pain. Cutting or other self-harming behavior may provide temporary relief or have some other meaning that needs to be understood. Self-descriptions as ‘broken’, ‘dead’ or ‘empty’ are not unusual. Self-loathing is common (see here and here).
overwhelming psychic pain. Cutting or other self-harming behavior may provide temporary relief or have some other meaning that needs to be understood. Self-descriptions as ‘broken’, ‘dead’ or ‘empty’ are not unusual. Self-loathing is common (see here and here).
The outside view (of destructive behavior) and the inside view (of desperation for relief) both need recognition. The inside view needs understanding; the outside view needs transcending.
Ann Kennedy needed to understand why she was cutting before she could change her behavior. Her therapist needed to go beyond dismissing the cutting and burning as ‘attention seeking’ in order to support this change.
Symptoms
Lists of symptoms don’t make it clear who is saying what about whom. Many appear to reflect internal experience, but may be written from an expert standpoint.
Areas generally covered include relationships, sense of self, emotions, and impulsivity, and in the following synthesis from a number of sources, I have moderated some of the ‘outsider’ language (see, for example, here, and here).
Formal diagnosis involves assessment of severity, but does not require all symptoms to be present.
Relationships
- Unpredictable swings between love and hate
- Difficulties with trust and feelings of dependency
- High sensitivity to rejection or criticism
- Intense efforts to avoid abandonment
Sense of self
- Fragile sense of self

- Deep feelings of insecurity and loneliness
- Chronic feelings of emptiness and hopelessness
Emotions
- Intense anger and difficulty regulating emotions
- Stress-related paranoia or dissociative symptoms
- Overwhelming cycles of dysphoria, sadness, irritability, anxiety
Impulsivity
- Impulsive behavior in areas such as sex, substance use, spending
- Self-harm including cutting, burning
- Suicidality (10% with the diagnosis commit suicide; see here and here)
Models
Ann Kennedy’s story touches on most of the symptom areas, and also draws on more than one model.
The medical diagnostic model and the trauma model are major options, but narrative models also provide a means of moving beyond the language of ‘experts’ into that of the person themselves.
Medical diagnostic model: “What is wrong with this person?”
As a term, BPD fits a medical diagnostic model, in which the ‘condition’ is seen as an ‘illness’ associated with a ‘patient’. Information about a patient’s history may be collected but then compartmentalised from symptoms and treatment. Explanations for gender differences in diagnostic rates are likely to be biological rather than sociopolitical.
Trauma model: “What has happened to this person?”
Symptoms of BPD can also be understood as Complex Trauma Disorder. The trauma model considers underlying issues (such as abuse) that produce the symptoms (such as difficulties in relationships) and relates them to developmental history (including family history). Judith Herman, Bessel van der Kolk, and Babette Rothschild are key names.
Trauma does not have to be a catastrophic event or series of dramatic events. It can be any sort of experience that renders a person helpless or unsafe, highlighting lack of control and causing major distress (see here).
Narrative model: “What is this person’s own story?”
The medical diagnostic model and the trauma model are both ‘expert’ models that come with readymade discourses, which may (or may not) be relevant for particular individuals.
A third possibility is to understand what is going on for the person in their own language. Individual stories may include elements of one or both major models, may combine them in various ways, reject or accept one or both completely, and introduce new elements of understanding.
I’ve not come across anyone who has constructed their BPD diagnosis in quite the positive light of the above image, but it does make the point that asking people for their own stories can get beyond the expert mindset.
Ann Kennedy, for example, did not find the medical model useful, but a trauma model helped her make sense of her symptoms and experiences. Medication didn’t work, but talk therapy enabled her to reclaim her life and stop self-mutilating.
My experience of working with asylum seekers has been that healing from the violence and trauma in their backgrounds remains largely on hold until urgent needs for future safety are addressed. This barricade to healing is partly what makes it so tragic that our current policies and practices systematically retraumatise people over such an extended time.
Treatment/Recovery/Getting a life
In terms of treatment for BPD, there is (again) an ocean of material, but the navigation involved is less than simple.
- The first and obvious point is that there is no one-size-
 fits-all panacea.
fits-all panacea. - Public services that specialise in BPD are rare.
- Medication is not routinely recommended, and there is little evidence of effectiveness, although it may be prescribed for some symptoms including depression, anxiety, and mood swings.
- If self-harm, suicidality, and impulsivity are creating safety concerns, Dialectical Behavior Therapy, developed by psychologist Marsha Linehan (who describes herself as having BPD) is widely recommended. (See also, DBT Self Help).
- Safety, and hope for the possibility of recovery are basic prerequisites. The encouraging message from several sources is that recovery is possible, as Ann Kennedy’s story has also shown.
- Beyond safety, and the need for hope, the challenge is to find the best fit between the person and what is available in terms of healing. Finding a philosophical match on issues raised in this post (about the gendering of the diagnosis, role of developmental history, importance of insider-outsider viewpoints, and preference for practice models) may repay effort.
- Encouraging people to ‘shop around’ can seem dubious advice, given that it takes energy which may well be lacking at crucial times. However, if the process (as in Australia) is to obtain a referral from a general medical practitioner, then being able to instruct that person is a good start. It should at least be unnecessary to persist with a referral that is not working. Ann Kennedy’s life might have improved earlier and faster if she had found her treatment-of-choice as a young adult rather than in middle age.
Conclusion
Borderline Personality Disorder is a medical-sounding term, applied as a diagnosis to experiences, emotions, and behaviors that are painful for the person and distressing for onlookers. As a term, it masks the gendered nature of the diagnosis and developmental histories behind it. Alternative ways of understanding the symptoms include medical, trauma, and narrative models, and finding the best fit between person, practitioners, and philosophical positions is a starting point for recovery.
Life can be understandable and satisfying, as Ann Kennedy notes, and holding that belief is a key to healing. Choosing professional help carefully, as she advocates, could pre-empt dead ends.
Scroll down to leave your comments…Joan Beckwith
For additional posts on issues of mental health click here
Social justice is for everyone (previously 2020socialjustice) is also on Facebook (click here)
And Twitter (click here)





Hi Joan,
My early childhood involved every type of the usual abuses against children, phyical, emotional, psychological and sexual. I was also abandonded by my parents at age 18 months and 5 yrs old. 8 months seperation each time. This was exacerbated by a psychopath who enthralled me at thirteen, married me at 18 and abandoned me at 26. During that marriage I had 2 stillborn daughters and was then referred to Dr Harry Bailey for PND. Pressure to have a lobotomy, huge amounts of drugs and deep sleep at Chelmsford Hospital followed. I now consider that my first husband and Bailey set out to murder my soul if not my body.
I have been diagnosed with – Bi-Polar type 2.
Major Depression
Complex PTSD
BPD
DID
The last 3 diagnoses I received after 1996. In 1995 I married my present husband and sought therapy because I was finding trust and abandonment issues rearing their heads and I wanted to be able to love him in a healthy and more positive way.
I spent the next 12 years in therapy with a woman psychiatrist. Three sessions a week of 90 minutes duration and then was terminated as untreatable. During those years I became very unwell and submitted to ECT and drug therapy which only served to worsen my symptoms.
I have since seen 3 psychologists for short periods of time but every time I end up getting very angry with them as they simply had no idea, even though they were very conversant with the Trauma Model.
Looking back over my life, I am now 69, I manage much better when I am not seeing anyone. I think that any medical professional whether they are involved in treating physical or mental issues triggers something very negative in me and I end up with BPD symptoms that normally lay dormant.
My husband and I have a loving and accepting relationship which has provided me with a stable home life and emotional support. It is not a one way street.
I have always had a strong sense of justice, even as a young child. This grew with my involvement with the women’s movement in London between 1976 and 1982 and many years working in women’s refuges in Australia plus my continuing political awareness and activism. I graduated with a Law degree in 1994 but never practised as I could not bear lawyers and came to see the Law as a tool used against our most vulnerable citizens and a weapon for the wealthy.
The things that trigger what some would see as BPD symptoms are any involvement with medical personel and injustice, particularly “blaming the victim”. I become full of rage and verbally aggressive. As I find this stressful and counter productive, I now avoid most social contact.
Despite living through times when despair ruled and all that entails I have enjoyed many wonderful times and a few deep friendships. I have accepted that I am different from most people in many ways, some innate and some as a result of my life’s experience. A couple of years ago I was diagnosed with high functioning Asperger’s which has made sense of much of my life, plus I now have the know how to avoid or deal with triggers.
I hope you do not mind me writing to you but I believe that some of what are considered to be BPD symptoms are normal responses to an insane world.
Lily.
Tw
HI Lily,
Thank you for writing. I very much appreciate hearing from you. It’s remarkable (in a non-positive way) when the people and processes that are meant to help instead reproduce the effects of the historical harms. Clearly counterproductive, which is appalling, but makes the life you describe having built, and the achievements along the way all the more remarkable (in a positive way).
I completely agree with your final comment, about normal responses to an insane world, one that can be incredibly toxic at a personal level.
I wonder if you have any thoughts about what might have been useful earlier in your life that might have actually helped you get through to where you are at now but with less wear and tear?
A relevant blog, including link to a newsletter: http://www.borderlinemother919.com/2015/01/living-and-loving-someone-with.html
This is a message to Joan, not related to the above article. Having earlier commented on an article about the Australian Liberty Alliance, I was prompted to go to your “About” page and read your brief autobiography. Allow me to give you a glimpse of my own. I grew up in Hungary under Soviet communism following the war and left after the brutal crushing by the Red Army of the uprising against the system in 1956. The comrades imposed social justice on us while they blatantly revelled in luxurious privileges afforded to them, such as motor cars, often with drivers (at a time when in my rural provincial town only the local vet had a car previously, enabling him to visit farms), indecently generous income, travelling internationally, most often on state expense, having access to foreign currency and able to shop for western luxury goods in dedicated stores not available to lesser mortals, engaging in a variety of corrupt practices, such as arranging the purchase of land and the building of homes by visiting expatriate pocketing sizable commissions, ad infinitum. Such was the case in the Soviet Union ad all the other countries it was subjugating, while the economies of those countries were going ever further south. Such is the case today in communist China, economically ameliorated by selectively applying free market principles, so is in Cuba, multiplied exponentially in North Korea, unmistakable in Vanezuela and other socialistically inclined South American countries. Such is the historical reality of social justice. I know, the theory goes, it would work perfectly if people’s social consciousness were developed to a sufficiently high degree. That’s what the comrades were mouthing while enjoying the privileges of those more equal than the rest.
Media article (not particularly profound but came across it at around the time of publishing this post) talking about a crisis of mental health in young women, 18-34, and raising connections between social context of women’s lives, insomnia, violence against women, and symptoms of BPD.
http://thenewdaily.com.au/life/2015/09/08/female-mental-health-crisis/?utm_source=SilverpopMailing&utm_medium=email&utm_campaign=20150909%20The%20New%20Daily%20(1)&utm_content=&spMailingID=23451013&spUserID=MTAyODk0Mjk5NTIwS0&spJobID=640806216&spReportId=NjQwODA2MjE2S0
And here is another article, this one raising the issue of “the missing middle” in mental health treatment (in general, but with relevance to those diagnosed with BPD) which identifies a gap between acute hospital care and referrals through the “Better Access” program to (mainly) counselling services. Community mental health services, including those that provide social support, receive “only around 7% of Australia’s mental health budget.”
https://theconversation.com/from-asylums-to-gp-clinics-the-missing-middle-in-mental-health-care-46345?utm_medium=email&utm_campaign=Latest+from+The+Conversation+for+September+16+2015+-+3401&utm_content=Latest+from+The+Conversation+for+September+16+2015+-+3401+CID_96f711658f4f84f02e8edcdd1d08468c&utm_source=campaign_monitor&utm_term=From%20asylums%20to%20GP%20clinics%20the%20missing%20middle%20in%20mental%20health%20care
And here is another one (that came out after publishing the post) about the (disputed) use of drug treatments with those diagnosed with BPD.
http://www.madinamerica.com/2015/09/drug-treatment-for-borderline-personality-disorder-not-supported-by-evidence/
Thank you for this. As a counsellor for many years in women’s health centres and working in a narrative model and extensively with survivors of trauma I found that BPD was so often the ‘scrap heap’ the one stop diagnosis that so many women received and were then placed in the ‘too hard basket’. I watched many women reclaim their lives with understanding of where the pain came from, with developing the skills to manage emotional dysregulation and with the development of a new story for themselves. I asked one of my clients once (permission to use this given) how she would define her problem and she said ‘pile of shit in my life disorder’. This is still my favourite diagnosis. Another client once defined ‘BPDO’ as ‘the bitch pissed the doctor off. I have been privileged to work with many women claiming their lives back from a nightmare childhood and I thank you on their and my behalf for this article.
I love both the reconstructions you cite (‘pile of shit in my life disorder’ and BPDO ‘bitch pissed the doctor off’) and the combination of them pretty much encapsulates the ‘insider-outsider’ distinction as well. If my post had not already been way too long for a blogpost I would have liked to explore renaming possibilities, so thanks for raising the idea, and thanks to the women who have shared their versions.
It’s always good to hear about what is possible through the kind of work you describe, and of course it would be even better if the journey could be short-circuited to bypass the time spent in the ‘too hard basket’.
As I’ve said, this post took a very long time in the making, and you would, I think, understand why. I had to start from a point (BPD) that I wanted to critique, but starting with it also felt potentially like giving it substance that it doesn’t have. A bit brain-hurting. Never mind, I’m glad you find the end result valuable…Joan Beckwith.
I found the gendered traits of NPD and BPD to be really interesting and something I will look into further. Good post, thanks Joan for the brain food.
The landmark book for me around the social construction and gendering of diagnoses was probably Paula Caplan’s (1995) “They say you’re crazy” in which she also proposed a diagnosis she called DDPD (Delusional Dominating Personality Disorder) which was intended to reflect hegemonic masculinity. It was never taken seriously by the DSM establishment, but did provide “brain food”. Thanks for your comments, Pheebz…Joan Beckwith.
The male as judge, and marker of “normal”
And holding the sociopolitical power to enforce the judgment thus perpetuating the status quo.
Hi Joan,
Thank you sooo much for this post.
Absolutely, people who are suffering emotional/psychological distress, who end up with diagnostic labels such as ‘BPD’ and many other ‘diagnostic labels’ including ‘schizophrenia’, more often than not have a trauma history. And you are right, trauma can be anything, from ‘the obvious traumas’ that immediately spring to mind, to the trauma of having a mum who is depressed or grieving or overwhelmed when their child is born, or even the trauma of being bullied at school. People with a trauma histories CAN be helped via many of the ‘transformative therapies’.
I’d recommend a book to clients and therapists, by Bessel van der Kolk, called: The Body Keeps The Score, published this year, 2015. He talks about the various ‘transformative’ therapies, that actually help ‘unlock’ synapses in the brain that ‘fire and wire together’. We used to think this was not possible. We now know that it is.
Thank you Joan for highlighting this issue.
I hope that people who have various ‘diagnoses’ who have a history of trauma find their way to a therapist who uses one of the ‘transformative’ therapies.
Best wishes,
Mary
Thanks for your comments, Mary. Thanks, also for the mention of the new book by Bessel van der Kolk, which I have so far only seen reviewed (link following in case it is useful to others). He and colleagues have made amazing contributions over a very long time, and one of his earlier works “Traumatic Stress” (1996) was outstanding in its time…Joan Beckwith.
http://www.madinamerica.com/2015/04/psychiatry-must-stop-ignoring-trauma-dr-bessel-van-der-kolk/
Hi Joan,
thanks for this article! I have Borderline Personality Disorder and I agree it is very treatable. The very best description I was given of BPD is that it is the adult result of the child’s experiences.
I did find that antidepressants mostly did not work for me, only once about five years ago did any antidepressant work in a positive way.
The very best treatments were talk therapies and in particular Cognitive Behaviour Therapy.
Looking at my core beliefs and looking back to where they came from and learning to create new beliefs for me, and in fact learning accurate descriptions of things that I had experienced changed how I look at myself, how I feel about myself, and changed my self talk.
I had tried in the past changing self-talk, tried meditation, yoga, but all of those things was like putting a band aid over a large abscess. CBT helped me to look at what had created the abscess and then to deal with it, and after that was done I found things like meditation, yoga, affirmations, and positive self-talk more helpful
I found that I still have BPD, I still struggle with some aspects of it, but have also learned that I can in fact live with it.
Having an associate who is a psychologist I was taken aback when he announced, “I don’t know why anyone would have diagnosed you with BPD. You do not present that way to me!” I was about to describe my struggle to him and reaffirm my BPD, I felt the need to prove it, but I took a breath looked him in the eye and said. “Thank you. I will take that as a compliment on all of the hard work I have done!”
Thanks for your comments, Cheryl, which I much appreciate. Positive stories are good to hear in their own right and also potentially hugely valuable for others who might still be looking for the light at the end of the tunnel. Your comment “I have learned that I can in fact live with it [BPD]” sounds like an anchor to return to in harder times, and a milestone achievement in the recovery journey. Best wishes and thank you again for taking the time and trouble to comment and share your experience…Joan Beckwith.
Thank you
You are most welcome.